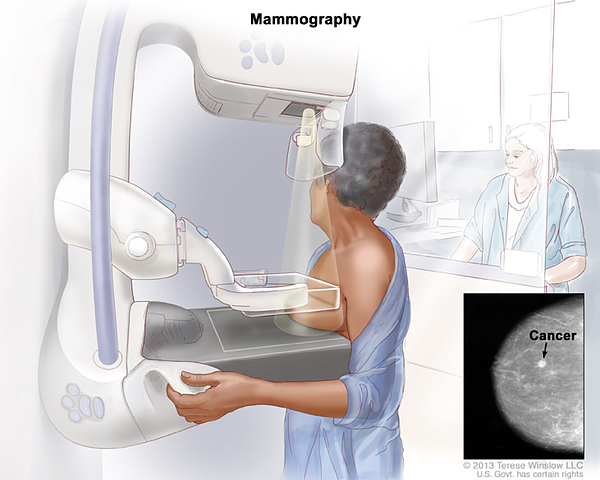
Mammography
Mammography
Why it is essential in the early detection of breast cancer?
The primary imaging modality for screening asymptomatic women is mammography. During mammography, the breast is compressed between plates to reduce the thickness of the tissue through which the radiation must pass, separate adjacent structures, and improve resolution. On screening mammography, two views of each breast are obtained, mediolateral oblique and craniocaudal. For further evaluation of abnormalities identified on a screening mammogram or of clinical findings or symptoms, diagnostic mammography is indicated. Magnification views are obtained to evaluate calcifications, and compression views are used to provide additional detail when a mass lesion is suspected.
Screening vs Diagnostic Mammograms
When a mammogram is used to detect cancer in women before they have any signs or symptoms of the disease, is it called a screening mammogram. Screening mammograms consist of two images of each breast, and detect lumps or other abnormalities.
Diagnostic mammograms are used after a lump or other symptoms of the disease have been found. It is also used if it is difficult to see breast tissue in a screening mammogram due to certain circumstances, such as the presence of breast implants. Diagnostic mammography consists of more x-rays than screening mammography and therefore takes longer to complete.
Women should begin scheduling their annual mammograms at the age of 40.
Mammographic Findings
Mammograms are read by radiologists. Radiologists are doctors who are specifically trained in diagnosing and treating diseases and injuries by using imaging techniques such as x-rays.
There are different types of signs your doctor will look for while looking at your mammogram:

Calcifications
Calcifications are tiny calcium deposits within the breast tissue. They look like small white spots on a mammogram. They may or may not be caused by cancer. There are 2 types of calcifications.
Macrocalcifications
Macrocalcifications are larger calcium deposits that are most likely due to changes caused by aging of the breast arteries, old injuries, or inflammation. These deposits are typically related to non-cancerous conditions and don’t need to be checked for cancer with a biopsy. Macrocalcifications become more common as women get older (especially after age 50).
Microcalcifications
Microcalcifications are tiny specks of calcium in the breast. When seen on a mammogram, they are more of a concern than macrocalcifications, but they don’t always mean that cancer is present. The shape and layout of microcalcifications help the radiologist judge how likely it is that the change is due to cancer.
In most cases, microcalcifications don’t need to be checked with a biopsy. But if they have a suspicious look and pattern, a biopsy will be recommended to check for cancer.
A mass is a region in breast tissue that looks abnormal.
A mass is the same as a lump or a tumor. With or without calcifications, it’s another important change seen on a mammogram. Masses can be many things, including cysts (non-cancerous, fluid-filled sacs) and non-cancerous solid tumors (such as fibroadenomas), but they may also be a sign of cancer.
Cysts are fluid-filled sacs. Simple cysts (fluid-filled sacs with thin walls) are not cancer and don’t need to be checked with a biopsy. If a mass is not a simple cyst, it’s of more concern, so a biopsy might be needed to be sure it isn’t cancer.
Solid tumors can be more concerning, but most breast tumors are not cancer.
A cyst and a solid tumor can feel the same. They can also look the same on a mammogram. The doctor must be sure it’s a cyst to know it’s not cancer. To be sure, a breast ultrasound is often done because it is a better tool to see fluid-filled sacs. Another option is to use a thin needle to remove (aspirate) fluid from the area.
If a mass is not a simple cyst (that is, if it’s at least partly solid), more imaging tests might be needed to decide if it could be cancer. Some masses can be watched over time with regular mammograms or ultrasound to see if they change, but others may need to be checked with a biopsy. The size, shape, and margins (edges) of the mass may help the radiologist decide how likely it is to be cancer.
Breast Density is based on how the different types of tissue in your breast are distributed. Dense breasts are not always abnormal, but it may be linked to a higher risk of developing breast cancer. Dense breasts can make it more difficult to see abnormal spots in mammograms, sometimes additional tests may be needed to determine if a woman is at risk for having or developing breast cancer.
Having a record of your previous mammograms is very important. It can help your doctor see the changes your breast tissue has gone through.
Mammographic Findings
On the day of your mammogram you should:
- Wear a comfortable two-piece outfit.
- Do not use deodorant or any products which may contain talcum powder or lotion.
During your mammogram:
- You will be asked to undress from the waist up and put on a gown.
- Once the radiologist is ready to see you, you will go to the mammography room and disrobe.
- Your breast is then placed on a special platform and slowly compressed until it is flattened.
- You may feel discomfort or pressure for several seconds, until your breast is released.
- The procedure is repeated until each breast is imaged twice from two different angles.
- The entire process of getting a mammogram generally takes about 30 minutes.
Mammogram Results:
- A radiologist reviews the images and sends the results to your doctor's office.
- You should get your results within a week from your mammogram appointment.
- If an abnormality is found, more imaging or additional tests such as a biopsy may be needed.
Detecting breast cancer as early as possible is critical to survival. Having a mammogram may be the first step in diagnosing breast cancer. Get checked!
References
Sabiston Textbook of Surgery