Colon Cancer
Colon cancer is a disease in which malignant (cancer) cells form in the tissues of the colon.
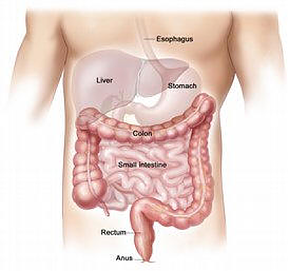
The colon (also known as the large intestine) is about five to six feet long, beginning at the cecum and ending with the anus. The last five to ten inches of the colon is called the rectum. Cancer located in the rectum is called rectal cancer, and cancer located in the rest of the colon is colon cancer. Colorectal cancer (CRC) is the term referring to both cancer types.
Colorectal cancer occurs when abnormal cells form tumors in normal tissues of the intestines and digestive system. The exact type of “colon” or “rectal” cancer depends on where the abnormal cells first began and how fast they grew and spread. The main differentiator between these two cancers is where the tumor first forms — in the rectum or in the rest of the colon.
CRC may not show any symptoms at first, but as the tumor grows, it can disrupt your body’s ability to digest food and remove waste. This causes potentially severe bowel and abdominal problems.
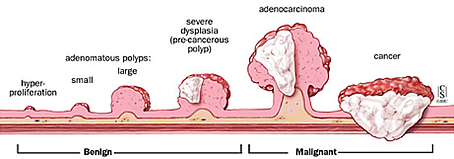
POLYPS AND HOW THEY GROW
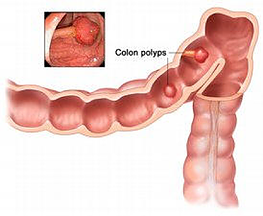
A colon polyp is a small growth found on the inside of the colon. Most polyps grow on the end of a stalk, somewhat like a mushroom. Although, some polyps, known as sessile polyps, can lie flat against the wall of the colon.
When it comes to polyps, you’re better safe than sorry. When a polyp gets larger than the eraser on the end of a pencil (five millimeters) its cells can gradually become cancerous. Not all polyps will become cancer, but it is important to remove them all to block the possibility.
Age and health history can affect the risk of developing colon cancer.
Risk factors include the following:
- Age 50 or older.
- A family history of cancer of the colon or rectum.
- A personal history of cancer of the colon, rectum, ovary, endometrium, or breast.
- A history of polyps in the colon.
 .
.
Polyps in the colon. Some polyps have a stalk and others do not. Inset shows a photo of a polyp with a stalk.
- A history of ulcerative colitis (ulcers in the lining of the large intestine) or Crohn’s disease.
- Certain hereditary conditions, such as familial adenomatous polyposis and hereditary nonpolyposis colon cancer (HNPCC; Lynch Syndrome).
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) depends on the following:
- The stage of the cancer (whether the cancer is in the inner lining of the colon only, involves the whole colon, or has spread to other places in the body).
- Whether the cancer has blocked or created a hole in the colon.
- The blood levels of carcinoembryonic antigen (CEA; a substance in the blood that may be increased when cancer is present) before treatment begins.
- Whether the cancer has recurred.
- The patient’s general health.
Treatment options depend on the following:
- The stage of the cancer.
- Whether the cancer has recurred.
- The patient’s general health
Knowing the signs and symptoms of colorectal cancer and understanding your risks may prevent this cancer from happening to you, or help you catch it as early as possible. Some early stages of colorectal cancer may not show any signs or symptoms. (Which is why screening is so important). If you have any signs or symptoms, do not ignore them. You need to tell a doctor.
All adults with an average risk of colorectal cancer need to undergo routine screenings starting at age 50. African Americans face a slightly higher risk and need to be screened starting at age 45. Those with a family history of colorectal cancer or any other risk factors should begin screening earlier than age 50 as well. If you see any signs or symptoms, you may need to be screened sooner.
Some people with colorectal cancer don’t experience any signs or symptoms. So be sure you’re aware of your body and talk with your doctor at the first sign of any of the symptoms below.
SYMPTOMS OF COLON AND RECTAL CANCER
Common symptoms of colorectal cancer may include:
- An ongoing change in bowel habits (diarrhea, constipation, or feeling that the bowel does not empty completely)
- Stools that are narrower than usual
- Blood (either bright red or very dark) in the stool (poop)
- Rectal bleeding
- Frequent gas pains, bloating, fullness or abdominal cramps
- Weight loss for no known reason
- Feeling very tired (weakness and fatigue)
These symptoms can vary based on the person. The signs and symptoms will also differ in severity based on the cancer’s location in the colon, size and growth. Some signs are mostly noticeable through changes with your digestive tract, but others can impact your entire body. Check with your doctor if you experience any of the above symptoms, regardless of your age.
NO SIGNS OR SYMPTOMS
It’s important to be screened for colorectal cancer, regardless of symptoms. Regular screening procedures can find polyps and remove them before the cancer can begin to grow, or they can catch early-stage cancer. If caught early, colorectal cancer is highly treatable and beatable. Some patients who undergo screening have a polyp removed, or cancer discovered, yet had no idea anything was wrong.
It’s not uncommon for individuals diagnosed in the early stages (stage I or II) to not experience any signs or symptoms of the disease. Signs and symptoms of early-stage colorectal cancer are not always obvious or visible. Oftentimes it’s only when colorectal cancer has grown into late-stage cancer or spread that signs and symptoms appear.
BLOOD IN THE STOOL
Not all cases of colorectal cancer will include rectal bleeding or blood in the stool; however, it’s a fairly common sign and should alert you that something’s not right. Tell your doctor. Rectal bleeding or blood in the stool should never be ignored.
Sometimes a blood test will reveal anemia (a low red blood cell count), which may indicate further screening is needed to discover the cause of your low blood counts. If you’re experiencing rectal bleeding, you should pay attention to the following factors and talk them through with your doctor:
- The color of the blood and/or stool
- Whether the blood is on or in the stool
- If the blood is on the toilet paper or in the toilet bowl
- How often the blood occurs
- If any other symptoms accompany the bleeding
CONDITIONS WITH SIMILAR SYMPTOMS
It’s pretty common for other conditions to cause some of the signs and symptoms of colorectal cancer. An infection, Crohn’s disease, ulcerative colitis and other GI issues can bring similar symptoms. It’s important to know your body and speak with your doctor to discover the cause of your symptoms and find treatment.
These conditions may also be risk factors for colorectal cancer. Your doctor can work with you to determine the best treatment plan for your current condition, as well as set up a prevention plan for a future case of cancer.
What causes colon and rectal cancers? Several factors may place you at a higher risk for colorectal cancer. If you have any of the following risk factors, speak with your physician about when you should undergo colon cancer screening.
RISKS YOU CANNOT CONTROL
Age
Over 90% of those diagnosed with colorectal cancer are over age 50. As we age, we are more likely to grow polyps which have the gene changes that turn normal tissue into cancer.
Personal History of Polyps or Cancer
If you have a personal cancer history of colon polyps or colon cancer, rectal cancer, ovarian cancer, endometrial cancer or breast cancer – you may be at an increased risk of colorectal cancer. You may want to talk with your doctor about whether genetic testing is appropriate for you.
Inflammatory Bowel Disorders (IBD)
If you’ve been diagnosed with an inflammatory bowel disorder such as ulcerative colitis or Crohn’s Disease, you are at a higher risk for colorectal cancer. Talk with your doctor about when your screening should begin.
Family History & Genetics
If you or a family member has a history of colorectal cancer, or colon polyps, you may be at an increased risk for colorectal cancer. Generally, screening for family members is recommended to begin 10 years prior to the survivor’s age of diagnosis. For example, if your loved one was diagnosed at age 52, family member screening needs to begin at age 42.
If your family has a known genetic syndrome, screening may be recommended earlier. Talk to your doctor if you have a family history of CRC. Even if not inherited, other genetic syndromes may increase your chances of colorectal cancer. Learn more about genetic risk factors.
RISKS YOU CAN CONTROL
Lifestyle
Low physical activity, obesity, smoking and heavy alcohol use are all linked to a higher incidence of colorectal cancer.
Diet
A diet high in red meats (beef, pork, lamb) processed meats and fats may all be linked to colorectal cancer.
PREVENTING CRC
While colorectal cancer screening is the most important way to prevent colorectal cancer, there are lifestyle changes that can reduce your risk for polyps and colorectal cancer. There is convincing evidence that the following strategies can decrease colorectal cancer risk:
- Don’t smoke
- If you do smoke, stop
- Increase your physical activity (get at least 150 minutes of moderate intensity or 75 minutes of vigorous intensity activity each week)
- Maintain a healthy body weight
- Avoid overall body fat, especially fat around your waist
- Reduce how much red meat and processed meats you eat
- Use alcohol in moderation
There is probable evidence that these additional strategies can reduce risk:
- Increase foods that contain dietary fiber
- Include garlic in your diet
- Drink more milk if you can tolerate it
- Add foods with calcium
- Use alcohol in moderation
Colorectal Cancer Under 50 Years Old
While over 90% of colon and rectal cancers are found in people over the age of 50, anyone at any age can get colorectal cancer.
People younger than age 50 need to protect themselves by knowing their family cancer history and their own medical history. Those with a family history of certain cancers, or with certain medical conditions, may need to begin screening earlier and be tested more often.
In addition, everyone, no matter how old they are, should be aware of the signs and symptoms of colorectal cancer. If experiencing any of these symptoms, talk to your doctor about the appropriate screening for you.
Most colorectal cancer is sporadic, which means it does not increase the risk of family members. Approximately 5-10% of all colorectal cancers are inherited, or caused by genetics.
Knowing if your cancer is inherited is extremely important because:
- It can help you understand the underlying cause of your cancer
- It can tell you if you are at risk for developing other types of cancers
- It can tell you if other family members may be at risk of developing cancer
RISKS OF INHERITING COLORECTAL CANCER
With inherited genetic abnormalities that increase the risk of colorectal cancer, there is generally a 50% chance that first-degree relatives (parents, siblings, children) inherit the same genetic abnormality and risk of developing cancer, however, other relatives could be at risk as well.
Knowing your family history can help you learn whether or not you should follow screening guidelines for higher risk individuals.
- Cancer at a young age (under age 50)
- Multiple primary cancers or bilateral cancer (occurs in both paired organs—e.g., both breasts, kidneys, ovaries)
- Two or more close relatives with cancer, especially of the same type
- A relative who is a known carrier of an inherited cancer susceptibility
- Concern about your family history of cancer
Our genetics resources will help you dig up, track and understand your family’s cancer history.
If you or your biological relatives meet any of the above criteria, you may be at high risk for colorectal cancer and could benefit from a cancer genetics evaluation. Talk to your doctor or call our toll-free Resource Line for resources. Visit our resource library for resources regarding genetics and family history.
GENETIC SYNDROMES LINKED TO CRC
There are several common genetic syndromes linked to colorectal cancer. This is not an all-inclusive list. View the National Cancer Institute’s information about additional genetic syndromes of colorectal cancer.
Lynch Syndrome
(aka hereditary nonpolyposis colorectal cancer)
Lynch Syndrome is a genetic syndrome that leads to an increased risk of colorectal cancer. Most of the time, the mutations that cause Lynch syndrome are located in the MLH1 or MSH2 genes, although there are others, and research continues to discover more. Only 3-5% of all colorectal cancer cases are linked to Lynch syndrome.
Signs of Lynch syndrome
Were you or a family member ever:
- Diagnosed with colon or rectal cancer before 50?
- Diagnosed with uterine/endometrial cancer before 50?
- Had 10 or more colon polyps over a lifetime?
- Two or more same-side family members diagnosed with colon, rectal or other Lynch-related cancers at any age (brain, breast, biliary tract, kidney, melanoma, ovarian, pancreas, small bowel, stomach, or uterine/endometrial)
The recommended age to start screening is age 20-25, or 10 years before the youngest case in the immediate family.
Learn more about Lynch syndrome from our partners at ThinkGenetic.
Familial Adenomatous Polyposis (FAP) and Attenuated Familial Adenomatous Polyposis (AFAP)
- Risk of developing colorectal cancer is about 100% if left untreated
- Average age at diagnosis: 39
- Average age of polyp formation: 16
People with FAP or AFAP will have an increased number of adenomatous colon polyps throughout their lifetime. The gene that is associated with both FAP and AFAP is APC (adenomatous polyposis coli).
The recommended age to start testing is between age 10-12.
Learn more about FAP from our partners at ThinkGenetic.
MYH-Associated Polyposis (MAP)
Mutations in the MYH gene (AKA: MUTYH gene), cause MAP. While the percentage of colorectal cancer that results from a MAP mutation is currently unknown, the risk of a person with MAP being diagnosed with colorectal cancer (and other cancers) is significantly increased.
Screening Is For Everyone
Almost all of the information you will read and the commercials you will see urge everyone to be screened at 50 years of age. For African Americans screening is recommended at age 45. Perhaps, even a few years earlier if you have a history of colon cancer in your family. There are even individuals and organizations that are lobbying to lower the standard age for which screening is recommended. The fact of the matter is ,this year approximately 13,000 young men and women will be diagnosed with colon cancer. That represents almost 10% of all new cases in the United States alone. We will not try to explain all of the economic, insurance, political, medical, or personal reasons why this is the case.
Does it matter what the statistics indicate if you, your spouse, your child, or someone you love or care about is diagnosed with colon cancer?
At any age:
If you experience any stomach discomfort, bleeding in your stool, or sudden weight loss, please contact your physician today.
People should talk to their doctor about starting colorectal cancer screening earlier and/or being screened more often if they have any of the following colorectal cancer risk factors:
- a personal history of colorectal cancer or adenomatous polyps
- a personal history of chronic inflammatory bowel disease (Crohns disease or ulcerative colitis)
- a strong family history of colorectal cancer or polyps (cancer or polyps in a first-degree relative [parent, sibling, or child] younger than 60 or in 2 or more first-degree relatives of any age)
- a known family history of hereditary colorectal cancer syndromes such as familial adenomatous polyposis (FAP) or hereditary non-polyposis colon cancer (HNPCC)
f you are not confident that your doctor is providing you with the correct information, or is not investigating the possibility of colon cancer immediately get a second opinion DEMAND THE PROPER DIAGNOSIS AND CARE. It’s you and your loved one’s lives at stake!
Colon and Rectal Cancer Screening
Beginning at age 50 (age 45 for African Americans), both men and women at average risk for developing colorectal cancer should use one of the screening tests below. The tests that are designed to find both early cancer and polyps are preferred if these tests are available to you and you are willing to have one of these more invasive tests. Of these the screening colonoscopy is the preferred test. Talk to your doctor about which test is best for you.
Tests that find polyps and cancer
- flexible sigmoidoscopy every 5 years*
- colonoscopy every 10 years
- double contrast barium enema every 5 years*
- CT colonography (virtual colonoscopy) every 5 years*
Tests that mainly find cancer
- guaiac-based fecal occult blood test (gFOBT) every year*,**
- fecal immunochemical test (FIT) every year*,**
- stool DNA test (sDNA), interval uncertain*
*Colonoscopy should be done if test results are positive.
**For both gFOBT and FIT based screening, the take-home method should be used and the manufacturer’s specimen collection instructions should be followed. A gFOBT or FIT done during a digital rectal exam in the doctor’s office is not adequate for screening.
If you cannot afford a colonoscopy (the gold standard for screening) or a barium enema combined with a sigmoidoscopy (almost as effective) see our page on getting help with screening.
Tests that examine the rectum, rectal tissue, and blood are used to detect (find) and diagnose colon cancer.
The following tests and procedures may be used:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Fecal occult blood test: A test to check stool (solid waste) for blood that can only be seen with a microscope. Small samples of stool are placed on special cards and returned to the doctor or laboratory for testing.
- Digital rectal exam: An exam of the rectum. The doctor or nurse inserts a lubricated, gloved finger into the rectum to feel for lumps or abnormal areas.
- Barium enema: A series of x-rays of the lower gastrointestinal tract. A liquid that contains barium (a silver-white metallic compound) is put into the rectum. The barium coats the lower gastrointestinal tract and x-rays are taken. This procedure is also called a lower GI series.
Barium enema procedure. The patient lies on an x-ray table. Barium liquid is put into the rectum and flows through the colon. X-rays are taken to look for abnormal areas.
- Sigmoidoscopy: A procedure to look inside the rectum and sigmoid (lower) colon for polyps, abnormal areas, or cancer. A sigmoidoscope (a thin, lighted tube) is inserted through the rectum into the sigmoid colon. Polyps or tissue samples may be taken for biopsy.
- Colonoscopy: A procedure to look inside the rectum and colon for polyps, abnormal areas, or cancer. A colonoscope (a thin, lighted tube) is inserted through the rectum into the colon. Polyps or tissue samples may be taken for biopsy.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope to check for signs of cancer.
- Virtual colonoscopy: A procedure that uses a series of x-rays called computed tomography to make a series of pictures of the colon. A computer puts the pictures together to create detailed images that may show polyps and anything else that seems unusual on the inside surface of the colon. This test is also called colonography or CT colonography.
A New Option for Colon Cancer Screening
Cologuard is a noninvasive test for colon cancer screening that identifies altered DNA and/or blood in your stool, which is associated with the possibility of colon cancer or precancer. Approved by the FDA in August of 2014, Cologuard was developed by Exact Sciences, in collaboration with researchers at Mayo Clinic. In a study of 10,000 people of average risk for colon cancer, Cologuard found 92% of cancer. Cologuard does produce false-positive results. In the clinical study, 13% of people without cancer or precancer tested positive. Cologuard must be ordered by a physician, and any positive result should be discussed with your doctor and be followed by a diagnostic colonoscopy. www.cologuardtest.com
Colonoscopy Coverage Under the Affordable Care Act
With the passage of the Affordable Care Act all individuals are required to have medical insurance. Every insurance plan must meet certain minimum requirements for what is covered. Colonoscopy coverage is a requirement for every plan going forward.
In general:
1. Colonoscopies performed as a routine screening are covered after age 50.
2. Normal copays would apply for colonoscopies performed for diagnostic reasons (for example, to find out the reason for rectal bleeding or other symptoms).
3. In both cases, there may be other charges, so it is important to contact your insurance provider before the procedure.
If you have a new health insurance plan or insurance policy beginning on or after September 23, 2010, colorectal cancer screening for adults over 50 must be covered without your having to pay a copayment or co-insurance or meet your deductible. This applies only when these services are delivered by a network provider. If your plan started before September 23, 2010, the rules about insurance coverage are covered by state laws, which vary, and other federal laws.
Even for routine screening colonoscopies, there may be other charges. For example, you may have to pay part of the anesthesiology charges. Check with your insurance provider before your procedure to confirm what is covered under your policy.
The bottom line? It is important to do your homework ahead of time so you don’t get any surprise bills, but don’t let this deter you from scheduling a colonoscopy. A colonoscopy can find non-cancerous colorectal polyps and remove them before they become cancerous. If colorectal cancer does occur, early detection and treatment dramatically increase chances of survival. The relative 5-year survival rate for colorectal cancer when diagnosed at an early stage before it has spread is about 90%.
The wall of the colon and rectum is made up of layers of tissues. Colorectal cancer starts in the inner layer and can grow through some or all of the other layers. It can also spread to other parts of the body.
Once colorectal cancer is detected, additional tests such as X-rays, CT, MRI and PET scans are performed to determine how far the cancer has progressed. This process is called staging. The stage of the disease greatly influences both treatment and survivability.
According to the American Cancer Society, the most commonly used staging system for colorectal cancer is that of the American Joint Committee on Cancer (AJCC) also known as the TNM system. This system describes:
- The Tumor – how far it has grown and whether or not it has grown into nearby areas
- Lymph Node involvement
- Metastasis – the spread of the cancer to other parts of the body
Numbers following each of these letters indicate their severity. This information is used to determine which stage the cancer is in. The stage is identified by the Roman numerals I through IV. These numbers may be further subdivided using letters A, B and C. In general, stages mean the following:
Stage 0: The cancer is contained to only the innermost lining of the colon or rectum.
Stage I: The tumor has grown into but not through the inner wall of the colon or rectum.
Stage II: The tumor extends farther into, or may have passed through the wall of the colon or rectum and may have invaded nearby tissue, but there is no involvement of the lymph nodes.
Stage III: The cancer has spread to nearby lymph nodes, but not to other parts of the body.
Stage IV: The cancer has spread to other parts of the body, such as the liver or lungs.
Recurrent: After a period of absence, the cancer has returned to the colon, rectum or another part of the body.
FACTORS THAT CAN AFFECT YOUR TREATMENT PLAN
- Stage of cancer
- Your overall health
- Whether or not the cancer has blocked the colon or made a hole in the colon wall
- Whether or not surgery completely removed the tumor and all metastatic tumors
- Specific tumor type, defined by laboratory tests known as biomarkers
- Your personal preferences
Surgical
Surgery (removing the cancer in an operation) is the most common treatment for all stages of colon cancer. A doctor may remove the cancer using one of the following types of surgery:
- Local excision: If the cancer is found at a very early stage, the doctor may remove it without cutting through the abdominal wall. Instead, the doctor may put a tube through the rectum into the colon and cut the cancer out. This is called a local excision. If the cancer is found in a polyp (a small bulging piece of tissue), the operation is called a polypectomy.
- Resection: If the cancer is larger, the doctor will perform a partial colectomy (removing the cancer and a small amount of healthy tissue around it). The doctor may then perform an anastomosis (sewing the healthy parts of the colon together). The doctor will also usually remove lymph nodes near the colon and examine them under a microscope to see whether they contain cancer.
Colon cancer surgery with anastomosis. Part of the colon containing the cancer and nearby healthy tissue is removed, and then the cut ends of the colon are joined.
- Resection and colostomy: If the doctor is not able to sew the 2 ends of the colon back together, a stoma (an opening) is made on the outside of the body for waste to pass through. This procedure is called a colostomy. Sometimes the colostomy is needed only until the lower colon has healed, and then it can be reversed. If the doctor needs to remove the entire lower colon, however, the colostomy may be permanent.
Colon cancer surgery with colostomy. Part of the colon containing the cancer and nearby healthy tissue is removed, a stoma is created, and a colostomy bag is attached to the stoma.
- Radiofrequency ablation: The use of a special probe with tiny electrodes that kill cancer cells. Sometimes the probe is inserted directly through the skin and only local anesthesia is needed. In other cases, the probe is inserted through an incision in the abdomen. This is done in the hospital with general anesthesia.
- Cryosurgery: A treatment that uses an instrument to freeze and destroy abnormal tissue, such as carcinoma in situ. This type of treatment is also called cryotherapy.
Even if the doctor removes all the cancer that can be seen at the time of the operation, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to increase the chances of a cure, is called adjuvant therapy.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the spinal column, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas.
Chemoembolization of the hepatic artery may be used to treat cancer that has spread to the liver. This involves blocking the hepatic artery (the main artery that supplies blood to the liver) and injecting anticancer drugs between the blockage and the liver. The liver’s arteries then deliver the drugs throughout the liver. Only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on what is used to block the artery. The liver continues to receive some blood from the hepatic portal vein, which carries blood from the stomach and intestine.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells. There are two types of radiation therapy. External radiation therapy uses a machine outside the body to send radiation toward the cancer. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer. The way the radiation therapy is given depends on the type and stage of the cancer being treated.
Biologic Therapy
Biologic therapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or immunotherapy.
This summary section refers to specific treatments under study in clinical trials, but it may not mention every new treatment being studied. Information about ongoing clinical trials is available from the NCI Web site.
Follow-up exams may help find recurrent colon cancer earlier.
After treatment, a blood test to measure carcinoembryonic antigen (CEA; a substance in the blood that may be increased when colon cancer is present) may be done along with other tests to see if the cancer has come back.
Diagnosed with colon cancer or rectal cancer? We’re here to help. We can guide you through this disease. From diagnosis to post-treatment, we provide reliable, trustworthy information and resources that you can read and discuss with your doctor. All of our information is reviewed by distinguished members of our Medical Advisory Board.
Let us help you understand your diagnosis and your treatment options no matter what your stage or age. We’re here to explain colorectal cancer terms, offer advice from other cancer patients and provide free resources for you to download.